Refractive or vision correction surgery includes techniques which alter the eye's focusing power by changing its natural structures, eliminating the need for glasses and contact lenses. In the year 2000, almost 2 million refractive procedures were carried out worldwide, the vast majority (>90%) being performed using laser technology.
Excimer
Today's most advanced refractive surgical techniques are performed with the excimer (excited dimers) laser. The development of excimer lasers began in 1975, when investigators noted that under high pressure meta-stable rare gas atoms produce unstable compounds. These compounds rapidly dissociate to the ground energy state of the individual molecules with the release of an energetic ultraviolet photon. These molecules can be induced to produce light amplification by stimulated emission when they are excited by an electron beam; the ArF (argon-fluorine) molecule emits light with a wavelength of 193 nm. At this wavelength corneal tissue can be removed with extreme precision – about 0.25 µm of corneal tissue is removed with each pulse – and with minimal damage to the surrounding tissue (fig. 4). For myopic correction central tissue has to be removed causing a flattening of the cornea; for hyperopic correction peripheral tissue is ablated to cause central steepening of the cornea, and for astigmatism an elliptical shape is removed to make all meridians of the cornea equally steep or flat. Today, the two main techniques used to correct refractive errors by reshaping the cornea are photorefractive keratectomy (PRK) and laser-assisted in situ keratomileusis (LASIK).
With PRK, the superficial layer of the cornea, the epithelium, is removed mechanically, and then a specific amount of stromal tissue is ablated using an excimer laser. Until the epithelium is healed, which usually lasts 3–4 days, a protective soft contact lens can be placed on the eye and corticosteroid eye drops are administered for 3–6 months. Overall, the results for PRK have been acceptable and have improved with experience. Currently, PRK is in use for myopia of up to –6.0 dpt, for astigmatism, and for hyperopia of up to +5 dpt. Typical complications are over- and undercorrection, central scar formation (haze) and corneal infections. The wound-healing process is prolonged and stability is mostly not achieved before 6 months.
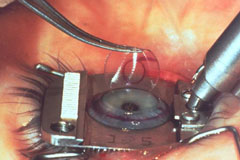
The second technique, LASIK, is a combination of a lamellar cut into the cornea and corneal stromal ablation using the excimer laser. The lamellar cut is produced with a microkeratome, cutting to a depth of about 120–160 µm, and leaving the flap attached to the cornea by a hinge (fig. 5). Excimer laser ablation is performed after the flap has been lifted up, leaving the stromal tissue of the cornea uncovered. After the ablation the flap is folded back onto the stromal bed, and within minutes the flap is attached by internal corneal forces and heals without sutures. The healing process is much faster after LASIK and a visual acuity of 20/20 (1.0) uncorrected on the first postoperative day is not rare. Correction of myopia up to –10.0 dpt, hyperopia up to +5.0 dpt and astigmatism of up to –5.0 dpt is possible and successful when all the contraindications for this type of procedure (thin corneas, extremely large pupil diameter and corneal pathology) are taken into consideration. Currently, other lasers like picosecond or femptosecond laser are being evaluated for their performance in intrastromal ablation or corneal lamellar incisions. New methods which correct the aberrations of the whole optical system, e.g. wavefront aberroscopy, are also being developed to increase the best corrected visual acuity of a human eye following refractive surgery.
Laser Thermal Keratoplasty
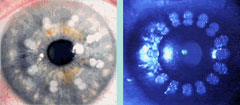
Laser thermal keratoplasty (LTK) is a promising new technique which uses laser energy to gently heat peripheral corneal tissue, producing a change in the cornea's refractive power. 16 or 32 spots are placed on the cornea in a symmetrical, circular fashion with high accuracy (fig. 6). Absorbed laser light increases the temperature of water and adjacent collagen fibrils, thus causing them to contract. The resulting tension produces a steepening of the anterior cornea over the optical zone, which is intended to correct hyperopic refractive errors. Currently, two types of thermal lasers are being used for hyperopic LTK: the holmium:yttrium aluminum garnet (Ho:YAG) laser (fig. 7) and the continuous-wave diode laser. Laser energy is delivered by either the noncontact or the contact mode. The procedure offers a solution for people over 40 who require glasses for reading, and corrections of up to +3.0 dpt of hyperopia can be achieved. In some patients, however, the result is not permanent and retreatment might be necessary.
The Beginnings
How Do Lasers Work?
Anterior Segment Surgery
Refractive Surgery
Pediatric Eye Surgery
Retinal Surgery
Conclusion
References
Biography
>> next