The use of lasers in treating anterior segment anomalies became popular in the last 30 years. As the anterior segment is easily accessible with conventional surgery, it took longer until laser surgery was used routinely in this part of the eye. Disorders for which lasers are used today are cataract (a clouding of the eye's natural lens which leads to blurred or decreased vision) and glaucoma (vision loss due to damage to the optic nerve, which is often caused by increased intraocular pressure).
Laser Surgery for Cataract
Cataract Removal
The current standard surgical technique to remove a cataract is phacoemulsification, introduced by Charles Kelman in 1967. A small incision of about 3 mm is made on the side of the cornea, the center of the lens is softened with ultrasound waves and removed, followed by the implantation of an artificial foldable intraocular lens. Removal of the human crystalline lens by laser (laserphaco) has been a dream for a long time and is currently in the developmental stage. Three different lasers are being used: neodymium:yttrium-aluminum-garnet (Nd:YAG) in the near-infrared energy range with a 1.064-µm wavelength, erbium: yttrium-aluminum-garnet (Er:YAG) with a wavelength of 2.94 µm, and yttrium-lithium-fluoride (picosecond laser). Each of these lasers holds great promise as a future clinical tool, but so far hard cataracts cannot be effectively removed and the surgical time needed to remove a standard cataract is comparable with that of phaco- emulsification. Although many ophthalmologists believe that some form of laser technology will be the future of cataract surgery, its putative advantages over standard ultrasonic methods still remain to be proven. More research is necessary to achieve safer and gentler cataract surgery.
Neodymium: YAG Laser
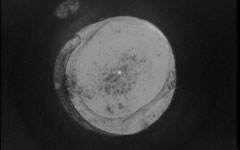
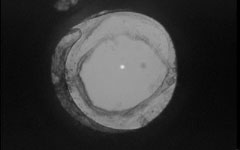
Secondary cataract formation (or after-cataract) is a significant late complication in people who undergo extracapsular cataract extraction, a procedure in which the surgeon removes the lens nucleus manually or with phacoemulsification (see above). In both types of surgery the posterior half of the capsule, the outer covering of the lens, is left behind. Following intraocular lens implantation, a formation of posterior capsular opacification (PCO) may develop (fig. 2a). The frequency of PCO is age-related. Almost all children develop PCO after extracapsular cataract extraction, whereas the incidence is much lower in adults. PCO decreases the visual acuity and therefore significantly diminishes the treatment success of cataract surgery. Patients with PCO require posterior capsulectomy, a procedure which removes the central part of the posterior capsule and instantly improves vision. Nowaday this opening of the posterior capsule (disruption of the posterior capsular bag membrane) is performed in a few seconds using an Nd:YAG laser. The procedure can be carried out on an out-patient basis at the slit lamp (fig. 2b). It has become the treatment of choice and has restored the visual acuity of millions of patients who were still unhappy after cataract removal.
Laser Surgery for Glaucoma
Lasers play an important role in modern-day treatment of glaucoma, where their main use is to lower intraocular pressure (IOP).
Argon Laser Trabeculoplasty
Argon laser trabeculoplasty (ALT) is a firmly established, well-tolerated procedure used to lower IOP in various types of open-angle glaucoma. It is performed by placing small, evenly spaced, nonpenetrating argon laser spots into the trabecular meshwork of the angle in the anterior chamber, which allow the aqueous humor to drain. A period of at least 4–6 weeks after ALT is required before the final result can be evaluated. Results show that ALT has managed to control IOP in 67–80% of eyes for 1 year, 35–50% for 5 years and 5–30% for 10 years.
Peripheral Laser Iridotomy
In 1857, von Graefe introduced surgical iridectomy for the treatment or prophylaxis of narrow-angle glaucoma. In 1956, Meyer-Schwickerath demonstrated that an iridectomy could be created without the need for an incision, using xenon arc photocoagulation. This method failed to gain popularity because of frequently occurring lens and corneal opacities. However, with modern lasers (argon and Nd:YAG), laser iridotomy has now essentially replaced surgical iridectomy in the vast majority of cases (fig. 3).
The Beginnings
How Do Lasers Work?
Anterior Segment Surgery
Refractive Surgery
Pediatric Eye Surgery
Retinal Surgery
Conclusion
References
Biography
>> next